IBD or Cancer? Diagnosing & Treating IBD vs Cancer
Laurie Goldstein, C.F.A.
Summary of what is discussed in this article:
Despite medical advances, there is still just one way to determine whether or not your cat has inflammatory bowel disease or some type of cancer, and that is with a biopsy. Your vet may not be familiar with recent research, but almost 50% of the time when symptoms of small bowel disease are present, the problem is actually cancer not IBD. But without that biopsy, we don’t know which it is. There is a new blood test that can rule cancer in – but it can’t rule cancer out. You need to know, if your vet was not clear, if this test (the TK-1) is negative, it does not mean your cat does not have cancer.
Finally, if your cat does have inflammatory bowel disease, it can become cancer. One of the very best ways to monitor your cat’s health status is to weigh your cat weekly. Cancer “eats” calories. Yes, the malabsorption of IBD often results in weight loss. BUT if you were able to stabilize your cat’s weight, or minimize the rate of loss, if the weight loss returns (or if the weight loss accelerates), you need to consult with the vet, as the cause may be that the inflammation has morphed into cancer.
The Diagnostic Process
“Here is a common, real-life scenario that I face in my feline-exclusive veterinary hospital nearly every week. A client comes into my practice with the complaint that their middle-aged to older cat has been losing weight for the past few weeks. I perform a physical examination, which unfortunately fails to reveal the cause of the weight loss. I inform the client that the top three common metabolic causes for weight loss are diabetes, hyperthyroidism, and chronic kidney disease, and that a few basic blood and urine tests should be able to determine whether the cat is afflicted with any of these three conditions. We run the tests. Everything comes back looking normal. At this point, the most likely cause of the weight loss is some type of gastrointestinal disorder. I recommend abdominal ultrasound to assess the gastrointestinal tract for abnormalities. We perform the ultrasound, which reveals that the intestinal walls are thicker than normal. This suggests that there is some kind of cellular infiltration going on in the walls of the intestines. If the cells that are infiltrating the intestine turn out to be inflammatory cells, we call this condition inflammatory bowel disease (IBD). If the cells are cancerous lymphocytes, we call this lymphoma. The only way to distinguish between these two conditions is to biopsy the intestinal tract. I tell my clients that we can obtain a biopsy in two ways – either by exploratory surgery or by endoscopy. Both procedures are costly and require anesthesia.” Dr. Arnold Plotnick DVM, blog post A Potential New Blood Test to Detect Cancer in Cats; Monday, December 16, 2013. (1)
The symptoms of small bowel disease can be caused by a number of things: parasites, allergies, intolerance/sensitivity to certain foods; bacterial infection, hyperthyroidism, diabetes, kidney disease, pancreatitis, exocrine pancreatic insufficiency (EPI) – all of these can (generally) be detected in blood work, where IBD or cancer cannot. The most common symptoms are diarrhea and/or vomiting, often in conjunction with weight loss. The symptoms of vomiting and diarrhea may not be constant, but come-and-go in cycles. An early symptom of small bowel disease includes regurgitating hairballs more than twice a month in any cat, and more than once every two months in short-haired cats. (2)
With blood work and a fecal, your vet can rule out other causes of the symptoms of small bowel disease. Food allergies or sensitivities may be considered at that point. When this list has been exhausted, your vet may diagnose your cat as (likely) having IBD. But if your vet did not say “it may be IBD or lymphoma,” you either have a vet that isn’t current on the research in the area, or you have a very young cat (which doesn’t exclude cancer, but it does make it less likely).
In fact, there is only one way to confirm a diagnosis of IBD and ensure it isn’t cancer, and that is with a biopsy. Many choose not to pursue this option for many reasons, and we address that in this article. But if your vet did not tell you, you need to know: there is new research (2013 and 2015) with which many vets are not familiar. This research found that almost half the time, cats with small bowel disease do not have IBD, they have cancer. And that is now based on an examination of over 300 cats from 2008 – 2012. (3)
How IBD is diagnosed and why blood work cannot tell the difference between IBD and cancer
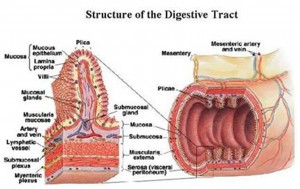
As explained by the All Feline Hospital, “IBD is kind of a swelling of the inner lining of the small intestinal tract. [Inflammation]. Normal intestinal tract lining looks kind of like the teeth of a comb. This lining, called the mucosa and submucosa, has peaks and valleys called villi and crypts to create the maximum amount of space for absorbing and digesting nutrients from your food. The lining is composed of immune cells, connective tissue, and bacteria to aid in digestion.
“With IBD, abnormal levels of immune cells fill in the crypts, effectively decreasing the amount of area for absorption, causing the lining to look more like waves, rather than jagged peaks and valleys. There are three primary types of immune cells that can do this, which are determined by the cause of the inflammation. These are lymphocytes (and in smaller numbers, plasma cells), eosinophils, and neutrophils.” (4)
Simply put, IBD is just what it says it is: inflammation of the bowels. This inflammation can be anywhere within the GI system, and often is in multiple places. Routine blood work may detect inflammation markers (or indications of bacterial infection) that can point to IBD, but there are no direct components of organ chemistry that can be measured to say “this is inflammatory bowel disease.” Nothing yet exists that can distinguish between inflammation caused by immune system cells or inflammation caused by cancerous cells.
Ultrasound
When the other causes of the same symptoms have been ruled out, an ultrasound is a very useful tool to see if there is inflammation in your kitty’s GI system, and if so, where. X-rays can be somewhat useful, but are not sensitive enough to distinguish early stages.
The value in having an ultrasound done is that it can see inflammation of the intestines or the organs (though it can be hard to detect inflammation in the pancreas without special training). An abdominal ultrasound can also see if there are swollen lymph nodes, or any lumps, bumps, masses – or lesions – that shouldn’t be there. But even with an ultrasound, if there are no masses and the main problem is thickened intestines, it cannot identify the cause of that inflammation. When there is inflammation, there is usually malabsorption of nutrients. Thus the next step is usually specialized blood work.
The GI Panel
Some vets skip the ultrasound due to the expense: it depends on our individual circumstances, vet preferences, and whether or not the vet has in-house equipment. But there are non-routine blood tests that can point to IBD – but they are expensive; they still do not provide a definitive diagnosis; they don’t differentiate between IBD or cancer either; and the same results can also be caused by pancreatitis, which is why many vets will recommend the ultrasound first. But these specialized blood tests do provide very important and valuable information. The four tests together are often referred to as the “GI Panel.”
Your cat must be fasted for 12 hours prior to the blood draw for the tests. The GI Panel typically includes four individual tests:
Blood serum levels of B12 (cobalamin);
Blood serum levels of Folate (another B vitamin);
Two tests check different aspects of pancreatic function:
The first check to see if the pancreas is inflamed (“pancreatitis,” measured by the fPLI);
The second checks to see if the pancreas is making the proper amount of pancreatic enzymes to effectively digest and metabolize food. If it isn’t, this is called Exocrine Pancreatic Insufficiency, “EPI,” and it is more common in cats than many vets think. (5) It is accurately diagnosed by this test, the fTLI.
When B12 and/or folate levels are low, these are a very good indication that there is some form of small bowel disease: it can be IBD, cancer, pancreatitis, or exocrine pancreatic insufficiency. When B12 is low and folate high, this is an indication of Small Intestinal Bacterial Overgrowth (SIBO).
Those two tests of pancreatic function can help pinpoint whether the problem involves the pancreas. Annoyingly, the finding that the pancreas is involved does not mean the intestines aren’t – which gets back to why the ultrasound is important in the diagnostic process. Many cats concurrently have either IBD or intestinal cancer and pancreatitis or EPI (or inflammation/infection in other organs, and depending on which ones, the diagnosis may be cholangeohepatitis or triaditis). The bottom line? Once the inflammation (or infection) sets in, it can spread to other organs if untreated, and our cats are masters at hiding discomfort – and their symptoms are so often ascribed to other causes.
My Vet Said there is a Test for Cancer!
There is a test that can determine there are rapidly dividing cells. It is called the thymidine kinase (TK-1) test. But as Dr. Brennan McKenzie points out in the SkepVet blog (Sep 11, 2014), “Cancers differ in their basic biology and behavior, so each requires a different approach to diagnosis.” (6) The TK activity, though, is especially prominent in lymphoma, which is the most likely form of cancer in feline intestines. (1) Unfortunately, the test is not very sensitive. Dr. Plotnick analyzes the data presented in the study of this test in cats:
“A significant number of cats with lymphoma (60%) did not have elevated serum TK levels. In addition, eight cats with inflammatory disease (including the five cats with pancreatitis) had TK levels above the reference range (i.e. they were in the lymphoma range). The fact that many cats with lymphoma had TK levels within the normal range means the test has low sensitivity: it will call a cat “normal” even though the cat truly has lymphoma. The test has a high specificity, however. In other words, if the serum TK level is high, it is very likely that the cat has lymphoma. Yet another way of saying this is: a normal TK level doesn’t mean the cat does not have lymphoma: it still might. However, a high TK level means the cat almost certainly has lymphoma.” [I note that 8 of 55 cats with inflammatory diseases were identified as having lymphoma that did not]. (1)
So – is this test worth having done in your cat? That depends on your situation. Clearly this test will NOT necessarily accurately diagnose cancer in your cat: if the TK levels are within the normal range, it does not mean your cat does not have cancer. But if your cat has lost weight, is not in the best of health, this test may be an option for ruling cancer in versus having a biopsy.
About Biopsies
There are two basic types of biopsies:
Endoscopic
Surgical
To understand the difference, take a look at this illustration. The two top layers of the intestines comprise the mucosa – but as you can see, there are quite a few more layers.
In the article, “Gastrointestinal Biopsies – Big Bite or Little Bite?” hosted at CriticalCareDVM (7) the advantages and disadvantages of each type of biopsy is outlined:
“Endoscopic Biopsies:
Advantages of endoscopic biopsies:
– Endoscopy is a relatively non-invasive procedure: although patients require general anesthesia, recovery from the procedure is rapid for most patients. As the endoscope is introduced to the body through the mouth and/or anus/rectum, there is no incision to heal.
– The inside lining (mucosa) of the esophagus, stomach, parts of the small intestine and large intestine (colon) can be visually inspected at the time of the endoscopy.
Endoscopic biopsies are obtained using small forceps passed down the endoscope instrument
Endoscopic biopsies can safely be obtained from the colon.
Endoscopic biopsy sites heal very quickly.
Endoscopic biopsies can be obtained in cats and dogs with low blood protein levels without increased risk of complications.
Disadvantages of endoscopic biopsies:
– Only a [very] limited portion of a dog or cat’s small intestine can be accessed using an endoscope. Most endoscopes are 1-1.5 meters (~40-60 inches) long while the small intestinal tract of dogs and cats is much longer. Thus this may be an issue if the disease only affects a certain area of the small intestine that is out of reach of the endoscope.
– Endoscopic biopsies come from only the innermost layer of the wall of the stomach and intestine (called the mucosal layer). This is an issue if the disease has caused changes in the deeper layers of these organs (called the submucosa, muscularis, and serosa).
– The quality of endoscopic biopsies can vary and is highly dependent on the expertise of the veterinarian performing the procedure. For this reason, it may be beneficial to work with board-certified veterinary internal medicine specialists who have undergone extensive and specialized training in endoscopic procedures.
Surgical (full thickness) biopsies:
Advantages of full thickness (surgical) biopsies:
– A sample that includes all the layers in the stomach or small intestine can be obtained. This means diseases that only affect the deeper layers of the stomach or small intestine can still be readily diagnosed.
– During surgery all three segments of the small intestine (called the duodenum, jejunum, and ileum) can be evaluated and biopsied. Furthermore any areas of bowel that are determined to be abnormal from the outermost layer (for example thicker than normal) can be specifically sampled.
– Biopsies can also be obtained from lymph nodes and other organs in the abdomen, most commonly the pancreas and liver, at the time of surgery. This is not possible during endoscopy, and may be important in some cats and dogs with cancer of the gastrointestinal tract.
Disadvantages of full thickness (surgical) biopsies:
– Although both methods of obtaining gastrointestinal biopsies require general anesthesia, recovery time is often longer following surgery than following endoscopy. Accordingly pets undergoing surgery are hospitalized longer compared to those who have an endoscopic procedure performed. Furthermore your pet’s exercise must be restricted until the surgery site has healed completely. If laparoscopy is possible, then recovery time may be reduced.
– Some dogs and cats with gastrointestinal problems have decreased blood protein levels. These patients have a higher risk of complications after full thickness biopsies, as the biopsy sites may not heal as efficiently as they should. These complications can be life-threatening and/or require a second surgery to remedy.
– Full thickness biopsies of the large intestine (colon) are rarely performed because there is a high risk of complications.”
As you can see, discussing which type of biopsy to use with your vet – or whether to have the surgery performed by a specialist – is important. If the disease is in the process of being diagnosed in its early stages, and your cat has not lost much weight, please bear in mind that the surgical biopsy has a much better chance of finding cancer (if it exists) versus the endoscopic biopsy.
PLEASE NOTE THIS IMPORTANT COMPLICATING FACTOR. If your cat has been treated for IBD with steroids, as steroids also function as chemotherapeutic agents, this use of steroids can make diagnosis of cancer, if it exists, difficult. Some specialists require that your cat be tapered off the steroids and steroid-free for six weeks prior to a biopsy. So if you have NOT yet started steroids, now may be the time to pursue the biopsy of choice versus trying to treat your cat first, because this can lower the probability of obtaining an accurate result from the expensive surgery (whether surgical or endoscopic).
Medical Treatment of IBD vs Cancer
It is outside the scope of this article to discuss IBD treatment. But a very short discussion of cancer treatments may help you have a better-informed discussion with your vet or specialist, because the use of steroids overlaps medical approaches to management of both IBD and cancer.
The two most common forms of gastrointestinal cancer in cats is lymphoma. There are two basic types of lymphoma:
Small cell (also called low grade), and
Large cell (also called high grade).
Both forms of cancer are usually a non-Hodgkins lymphosarcoma.
Small Cell Lymphoma
The most common form of intestinal cancer in cats is the small cell form of lymphoma, and the good news is it is very slow growing. It is treated with a combination of an oral chemotherapeutic agent, Leukeran (generic is chlorambucil), and a high dose of prednisolone (a glucocorticoid steroid) that is rather rapidly tapered down to a low dose, usually given every-other-day. There are two methods of dosing the chlorambucil: the most commonly prescribed is a lower dose every-other-day, sometimes tapered down to every third day. The dose schedule published in more current literature (8) is a larger dose administered once every two weeks. This must be compounded for cat-specific dose capsules. The prognosis with proper treatment is quite good (even better with early identification), and most cats tolerate the therapy well.
Large Cell Lymphoma
Large cell cancer can mass or be diffuse. This is a far more aggressive cancer. While treatment varies, it is typically a series of intravenous administrations of differing chemotherapeutic agents, typically the “CHOP” protocol. (9) Whether or not to pursue treatment is a very individual decision, based on the cost (usually around $150 – $200 per treatment, it often includes 4 to 16 treatments), the temperament of your cat to manage the visits, the treatment, and the drugs. This treatment approach is successful at putting the cancer into remission only about 50% of the time, and the average length of remission is, on average, 9 months. Approximately 15% of cats experience side-effects that result in stopping the therapy.
To Biopsy or Not? Treatment Options & Implications
As many pet parents opt not to put their cat through biopsies (though at IBDkitties, we suspect this is because many vets do not make it clear how often what they diagnose as “IBD” without that biopsy is actually cancer, especially in pets that are older when the symptoms of small bowel disease occur), by using prednisolone to treat your cat’s IBD, you are slowing down the rate of growth of cancer, if it exists. Unfortunately, there are many potential unpleasant side-effects with the use of steroids in your cat, one of the primary problems being the development of diabetes and/or pancreatitis.
Most vets treat IBD as a diagnosis of exclusion, and understand the substantial financial constraints in obtaining a definitive diagnosis via biopsy IF the GI symptoms appear prior to substantial weight loss and your kitty is in *reasonably* good health at the time of diagnostics. Recognizing that GI inflammation can morph into cancer, more vets are willing to treat cats for small cell lymphoma with chlorambucil when the symptoms of IBD become intractable with diet and steroid therapies, (8) despite no biopsy having been performed. It is best to discuss these alternatives and outcomes with your vet prior to the administration of even prednisolone, however, as that can confound biopsy results when or if you do decide to pursue that diagnostic avenue.
With the new TK-1 test, pet parents have an option to rule cancer in. Although the TK-1 test cannot identify whether the cancer is large or small cell (and a negative test does not mean your cat does NOT have cancer), if the test indicates a cancer is present, based on the probability of small cell versus large cell, some vets are willing to prescribe chlorambucil and prednisolone. If your cat responds, you can be reasonably assured you have the right treatment on board.
Remember: whether or not you decide to pursue therapy, whether for small cell or large cell, you can always stop, depending on how your cat reacts to treatment.
For Further Information on Small Cell Intestinal Lymphoma
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092124/
References
1. Plotnick A 2013. A Potential New Blood Test to Detect Cancer in Cats, Cat Man Do blog by Dr. Plotnick of Manhattan Cat Specialists, Monday, December 16, 2013. http://catexpert.blogspot.com/2013/12/a-potential-new-blood-test-to-detect.html
2. Norsworthy, Gary 2014. Chronic Vomiting in Cats isn’t Normal After All. Veterinary Practice News online, Jan 22, 2014.
http://www.veterinarypracticenews.com/Chronic-Vomiting-in-Cats-isnt-Normal-After-All/
3. Norsworthy G et al 2015. Prevalence and underlying causes of histologic abnormalities in cats suspected to have chronic small bowel disease: 300 cases (2008 – 2012), J Am Vet Med Assoc. 2015 Sep 15;247(6):629-35.
4. Knudsen S. Inflammatory Bowel Disease (IBD) handout, written for All Feline Hospital, Lincoln, NE.
http://www.allfelinehospital.com/inflammatory-bowel-disease.pml#
5. Carr, AP 2013. Exocrine pancreatic insufficiency in cats: More common than veterinarians think, DVM360 online, Mar 1, 2013.
http://veterinarynews.dvm360.com/exocrine-pancreatic-insufficiency-cats-more-common-veterinarians-think
6. McKenzie B 2014. Is There a Blood Test for Cancer in Dogs and Cats? SkepVet blog, September 11, 2014.
http://skeptvet.com/Blog/2014/09/is-there-a-blood-test-for-cancer-in-dogs-cats/
7. Dr. Fiona Park, guest blogger on CriticalCareDVM blog Because Pets Can Have Specialists Too, Gastrointestinal Biopsies – Big Bite or Little Bite? April 13, 2015. http://criticalcaredvm.com/gastrointestinal-biopsies-big-bite-or-little-bite/
8. Stein TJ et al 2010. Treatment of Feline Gastrointestinal Small-Cell Lymphoma With Chlorambucil and Glucocorticoids, J Am Anim Hosp Assoc. 2010 Nov-Dec; 46(6): 413–417. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092124/
9. Merck Veterinary Manual, Treatment of Canine Lymphoma.
http://www.merckvetmanual.com/mvm/pharmacology/antineoplastic_agents/treatment_of_canine_lymphoma.html
