By Marje Blaine
First and foremost, a diagnosis of feline diabetes is not a death sentence for your cat. With the proper insulin and diet, barring other serious illnesses/diseases, cats can live a very long time, be relatively healthy, and have a great quality of life with feline diabetes. Some cats are even able to go into remission and be insulin independent (i.e. not require insulin injections) although those kitties will always be diabetic and may, at some time in the future, again require insulin injections.
This topic will provide some basic information about feline diabetes and treating it and give links to where the caregiver (CG) can find help and additional information.
What is Feline Diabetes and what causes it?
It’s important to understand how the body functions normally with regard to sugar and insulin. In order for sugar to enter a cell to provide energy, it needs insulin. Insulin is made by beta cells in the pancreas. Sometimes the beta cells can become damaged by medications such as steroids, by a virus, infection, trauma, chronic inflammation, or too much carbohydrate consumption for too long. When the beta cells become damaged, they can no longer produce the amount of insulin needed to remove sugar from the blood and “escort” it into the cells for energy production.
When this occurs, the amount of glucose (sugar) in the blood increases and the other organs must work harder to remove the sugar from the blood. The liver, in particular, will try and remove the sugar for future use but if there’s still extra sugar, it enters the urine via the kidneys and then passes out of the body. Once the liver’s storage of sugar is full and the kidneys can’t process any more in the urine, then the circulatory system has to hold it and that is when high blood glucose numbers are seen.
Some of the major “culprits” which cause Feline Diabetes are use of steroids (e.g. for treatment of many conditions including IBD), diets which are too high in carbohydrates (specifically, dry food diets), and chronic infections/inflammation. While some cats’ blood glucose levels will drop back to normal once steroid use is discontinued or the high carbohydrate dry food is switched to a low carbohydrate wet food, most cats will require some insulin support. Some of them will only need it temporarily but some will require it permanently dependent on the degree of damage done to the beta cells and whether they can “recover” and begin to make their own insulin again in enough quantity so the cat no longer requires insulin shots.
The use of steroids is often indicated in the treatment of IBD. Steroids used in veterinary medicine are generally glucocorticoids. Glucocorticoids, which are “catabolic steroids”, counter the effects of insulin and increase glucogenesis through catabolism of proteins and fats. Catabolism occurs when larger molecules are broken down into smaller ones. Glucocorticoids also cause carbohydrates stored in the form of glycogen to be converted back to glucose and deposited into the circulating blood resulting in an overall effect of increasing the blood glucose. On a short-term basis, the natural insulin produced in the pancreas may be able to handle effects of steroids on blood glucose levels. However, diabetes is more likely to develop for cats that may be pre-disposed to diabetes or require long-term steroid use. If you are concerned about your cat developing Feline Diabetes due to steroid use, discuss it with your vet. However, keep in mind that treating Feline Diabetes is more manageable than treating IBD and there is always the potential that as steroids are decreased or eliminated, the Feline Diabetes may go into remission.
The two steroids that are often used for treatment of IBD are prednisolone and budesonide. Prednisolone tends to have more overall systemic effects while budesonide generally has less systemic effects and may be the better choice for cats that are pre-diabetic or diabetic as there is less potential for blood glucose to increase with the use of budesonide. However, it is important to note that every cat is different and the effects of either steroid on blood glucose will likely vary from cat to cat.
Symptoms of Feline Diabetes
Some of the symptoms (polydipsia and polyuria) of Feline Diabetes are similar to those of other conditions such as hyperthyroidism and acute or chronic kidney disease. Polydipsia (PD) is increased water consumption and polyuria (PU) is increase urine production. When the kidneys attempt to rid the system of excess sugar, they do it by increasing the amount of urine. In order to increase the amount of urine to rid the body of sugar, the body takes water from other tissues. This leaves the kitty feeling dehydrated because the tissues and cells need more water to work properly and so it drinks more. Diabetic cats also eat like they are starving. The cells are not getting the sugar they need to work properly and so the cells trigger an eating response since more food is more sugar. However, the problem is not a lack of food but a lack of insulin to get the sugar into the cells. It becomes a vicious cycle of more food putting more sugar in the cells, then the liver and kidneys working overtime to rid the body of the excess sugar, which leads to more urinating and more drinking. Diabetic cats will often become lethargic because the cells do not have the sugar they need to provide energy. They will also typically lose weight because the cat’s body will deplete any stored fat it has and then start breaking down muscle in attempt to gain energy and allow the body to function properly.
If the diabetes goes untreated, the body may start to produce ketones. Ketones are the waste products of fatty acid breakdown in the body, which occur when the cat burns fat instead of glucose. When present in the blood, the cat’s body tries to rid it of the ketones as quickly as possible by the kidneys filtering them out of the blood and excreting them into the urine. A further discussion of the danger of the presence of ketones is below under Diabetic Ketoacidosis.
Treatment of Feline Diabetes
While some instances of high blood glucose can be addressed through elimination of steroids and high carbohydrate diets such as dry food, in many cases, your veterinarian will want to start your cat on insulin therapy. Insulin is a hormone, not a medication thus the saying that “every cat is different” in its response to insulin therapy. Some cats may achieve regulation quickly while others might take longer. However, it is extremely important to note that if your cat is getting insulin, even if the glucose numbers still are high for a period of time, the kitty is getting better and its body is no longer “starving”. Achieving the correct insulin dose to bring the kitty back to normal blood glucose numbers might take time depending on how long the kitty had undiagnosed diabetes. But the fact that it is receiving insulin and that insulin is helping the body deliver sugar to the cells goes a long way towards the kitty feeling better and being better.
There are several types of insulin that work well in cats. These are discussed below with the “gold standard” insulins being listed first. This information is provided for you to use in discussions with your veterinarian.
Long Duration Insulins: The best insulins for cats today are actually human insulins and include Lantus (Glargine) and Levemir (Detemir). While these insulins work a little differently in the manner in which they deliver insulin to the body over a 12-hour period, they are both extremely effective in treating feline diabetes. Cats have a faster metabolism than humans; therefore, these insulins should be administered every 12 hours. There are rare instances where a cat has been on one of these insulins for some time and is close to going into remission and may only need one shot a day; however, the majority of cats require these insulins every 12 hours. If you are just starting your cat on insulin and the vet recommends one shot a day, it is wise to get another opinion as the vet might not understand the action of these insulins in cats. These two insulins are not “in and out” insulins such as the medium or short duration insulins and they cannot “yank down” high numbers. Therefore, it often takes time and patience to see a response but once the ideal dose is attained, these insulins are outstanding for their ability to provide long duration. The effects of the shots are cumulative which provides the body with a more consistent supply of insulin and the dose is typically based on the lowest number (nadir) achieved instead of the preshot blood glucose and dosing needs to be consistent over a period of time. Lantus and Levemir require prescriptions from your vet. These insulins do not onset immediately after the shot is given; Lantus onsets approximately two hours after the shot and Levemir approximately four hours after the shot.
Medium to Long Duration Insulins: Prozinc and Bovine PZI insulins are medium duration insulins designed for use in cats and, depending on the cat, the caregiver, the veterinarian, and the protocol followed, can be given every eight or 12 hours. Dosing is typically based on the preshot blood glucose value and doses can be changed each cycle, if warranted. Bovine PZI is no longer readily available and must be compounded through a compounding pharmacy. Due to this, there is concern with potential contamination; therefore, most veterinarians who use these insulins will prescribe Prozinc.
Short to Medium Duration Insulins: Insulins which fall in this category include Humulin/Novolin N (approximately 6 hours duration), Humulin/Novolin R (approximately 4 hours duration), Caninsulin and Vetsulin. It is important to note that some cats get much longer duration on these insulins (even up to 8-10 hours). These insulins tend to onset quickly (usually within one hour) after the shot and are quicker acting in bringing down higher numbers. They tend to be more “harsh” insulins in their ability to quickly drop the blood glucose and once the insulin has worn off, the blood glucose can also quickly rise.
Hometesting
Many veterinarians will tell a caregiver to not hometest their cat because the cat will become hostile and it is not necessary to test a cat at home. Nothing could be further from the truth. The American Animal Hospital Association (AAHA) strongly encourages hometesting. Hometesting allows a caregiver to do glucose curves at home, which provides more realistic numbers (and is less expensive) than glucose curves done at the vet’s office where stress is a factor. Hometesting will keep your cat safer and allow you to monitor numbers and avoid a symptomatic hypoglycemic episode (see “Dangers”) below. Cats should have their blood glucose checked before every single shot. This enables the caregiver to determine if it is safe to give the insulin shot and when the cat should be tested again.
Hometesting does not require the caregiver to purchase an expensive pet glucometer such as an Alpha Trak 2. While these meters are excellent and give the best indication of the cat’s blood glucose, they are costly. The test strips are also costly and not readily available. Most diabetic cat caregivers use human glucometers such as ReliOn Micro or Contour meters obtained at WalMart. These are inexpensive, as are the test strips, they are also readily available, and they require a very small sample size. Many other human meters such as Bayer Contour, Target Up and Up, and Accu-Chek (specifically Nano) are other examples of human meters which are cost-efficient and can be used to hometest. Hometesting allows the caregiver to learn their cat’s pattern on insulin and understand when the cat’s insulin onsets, when the cat reaches the peak action of the insulin (i.e. the lowest number which is the nadir), and the duration of the insulin for their cat.
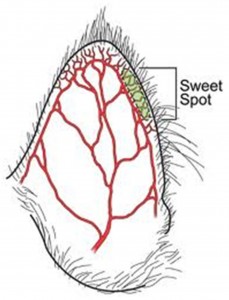 The other requirements for hometesting include test strips for the specific glucometer you are using, lancets and, if desired, a lancing device which typically comes with the purchase of a glucometer. Some caregivers prefer to freehand when testing rather than using a lancing device. Most caregivers obtain a very tiny sample of blood by pricking the very edge of the cat’s ear (see figure below) with a fine-gauged lancet (it is recommended to start with a 28g lancet and as the cat’s ear “learns” to bleed, use a finer gauge lancet such as a 31g or 33g). There are few nerves in this area of the ear and cats often tolerate testing using the edge of the ear very, very well and many will purr and even sleep through their tests! Learning to hometest takes a little patience on the part of the caregiver but it is well worth it to keep your kitty safe from blood glucose levels that are too low.
The other requirements for hometesting include test strips for the specific glucometer you are using, lancets and, if desired, a lancing device which typically comes with the purchase of a glucometer. Some caregivers prefer to freehand when testing rather than using a lancing device. Most caregivers obtain a very tiny sample of blood by pricking the very edge of the cat’s ear (see figure below) with a fine-gauged lancet (it is recommended to start with a 28g lancet and as the cat’s ear “learns” to bleed, use a finer gauge lancet such as a 31g or 33g). There are few nerves in this area of the ear and cats often tolerate testing using the edge of the ear very, very well and many will purr and even sleep through their tests! Learning to hometest takes a little patience on the part of the caregiver but it is well worth it to keep your kitty safe from blood glucose levels that are too low.
The following two instructional videos are provided to assist a caregiver in learning to hometest. Most cats will adjust to hometesting as Buddy shows in the first video.
How To Test Your Diabetic Cat’s Blood Sugar At Home
https://www.youtube.com/watch?v=_zE12-4fVn8&feature=youtu.be
How I test our cat’s Blood Glucose with an Alpha Trak II meter
https://www.youtube.com/watch?v=favfhB42AS4&feature=youtu.be
Insulin Dosing and Injections
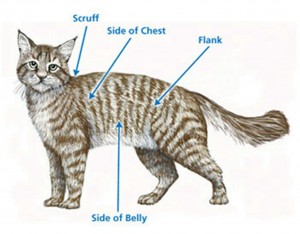
The starting dose of insulin depends on many things including the weight of the cat, the blood glucose level at time of diagnosis, the type of insulin being given, the approach to management of diabetes (e.g. using a tight regulation protocol as opposed to starting low and increasing the dose slowly, as may be required), and even whether the cat is eating dry food or wet food. Insulin injections are given subcutaneously and are often given in the scruff but may be given in other areas of the cat’s body as shown in the figure below. Typically, insulin absorption is slower in the scruff and faster in other areas.
Feeding the Diabetic Cat
Typically upon diagnosis, veterinarians will prescribe a prescription diabetes diet. Your cat does not need this expensive diet and will do much better on a non-prescription, low carbohydrate canned or raw diet. Since many cats that are diagnosed with Feline Diabetes are eating dry food, the first step is to slowly transition from a dry food diet to a low carb canned diet. Caution should be used because as the transition is occurring, the insulin needs will most likely decrease!!! It is extremely important to closely home monitor blood glucose levels while making the transition. Dr. Lisa Pierson has developed Food Nutritional Composition charts (http://www.catinfo.org/docs/FoodChartPublic9-22-12.pdf) that are extremely helpful in selecting low carb foods for the diabetic cats. Most diabetic cats will do well with a canned or raw diet, which is comprised of 4-10% calories from carbohydrates. Once the cat is slowly transitioned from dry to canned food and is doing well, then the caregiver can determine if raw food is appropriate for their cat and slowly transition to a homecooked or raw food diet. This is, in particular, important if the cat has IBD. Diabetic cats also do well with several smaller meals a day fed prior to the nadir of the insulin.
Dangers Associated with Feline Diabetes
Hypoglycemia: The most common and greatest danger to diabetic cats receiving insulin is symptomatic hypoglycemia or low blood glucose. Hypoglycemia can kill!! However, this danger can be greatly reduced if the caregiver is hometesting and has a hypoglycemia toolkit which includes high carbohydrate canned food and either syrup, karo, or honey. There are many symptoms of hypoglycemia and some cats will show none of them (another important reason to hometest) and some will show the most severe. Sudden ravenous hunger, shivering, and lethargy might be seen with mild hypoglycemia. Symptoms of moderate hypoglycemia may include disorientation, vision issues, poor coordination or staggering, restlessness, urgent meowing, or becoming aggressive. Severe hypoglycemia may result in convulsions or seizures and/or unconsciousness. A caregiver should immediately contact their vet or a veterinary emergency room if the cat is showing any signs of hypoglycemia.
Hyperglycemia: Prolonged hyperglycemia (or high blood glucose) can be a condition of grave concern although the results of prolonged hyperglycemia will not be seen as quickly as a short time of hypoglycemia. Cats who have prolonged hyperglycemia can, at the least, become insulin resistant so that it takes more insulin to start bringing the blood glucose down. Prolonged hyperglycemia can also affect body organs through glucose toxicity and, left untreated, may result in death.
Diabetic Ketoacidosis (DKA): It is imperative that caregivers of diabetic cats test the urine for the presence of ketones using Ketostix commonly found at pharmacies. If the Ketostix show even “trace” ketones, the vet should be immediately contacted as ketones can rapidly accumulate and “may” result in DKA, which requires emergency veterinary care and can be fatal. If the cat seems normal and is eating, some vets may elect to start the cat on subq fluids at home to address trace ketones. However, if your diabetic cat’s urine shows trace ketones, please do not attempt treatment at home without consulting your vet! The “recipe” for DKA is not enough insulin + infection present + inappetance. Symptoms of DKA include drinking excessive amounts of water or no water at all, not eating for over 12 hours, excessive urination, diminished activity, lethargy/depression, breathing quickly, dehydration, vomiting, and/or ketone odor (smells like nail polish remover) on the breath.
Resources
The information provided herein is just a quick overview of Feline Diabetes. Every caregiver when first faced with this diagnosis is in a state of shock and panic. However, the main point to remember is that feline diabetes is extremely treatable!! In fact, feline diabetes is much easier to manage than IBD.
The best resource for learning about Feline Diabetes is the Feline Diabetes Message Board. Not only is there a wealth of information located there, but there are extremely experienced and knowledgeable members who have been caring for diabetic cats 24/7 for months and years and there is always someone available for support and help. The caregiver can find information on insulins, protocols and approaches to insulin therapy, how to give shots, appropriate foods to feed, how to hometest and track the blood glucose on a spreadsheet, supplies needed, answers to likely all of your questions, and support from those who are dealing with feline diabetes now or who have dealt with it.
Feline Diabetes Message Board:
www.felinediabetes.com
AAHA Diabetes Management Guidelines for Dogs and Cats:
http://www.felinediabetes.com/AAHADiabetesGuidelines.pdf
Consumer Reports Best Glucometers (2013):
https://docs.google.com/file/d/0B9RKBhanggleTWhRTFVEc0xYbkk/edit
Feeding your Cat: Know the Basis of Feline Nutrition:
www.catinfo.org
Ketones, Ketoacisosis, and Diabetic Cats:
http://www.felinediabetes.com/ketones.htm
